Medically Reviewed by: Chris Duncombe, M.D.
We’ve all been prescribed antibiotics at one point or another. They can provide
The potential side effects, however, are another story.
Upset stomach, diarrhea, allergic reactions
The encouraging news is that probiotics can reduce the uncomfortable side effects of antibiotics and may also have a positive
In this article, we’ll show you how and why it’s beneficial to take probiotics while on antibiotics but first we’ll start with some information on antibiotics and probiotics as it’s important in understanding the overall topic.
Share this Image On Your Site
What Are Antibiotics?


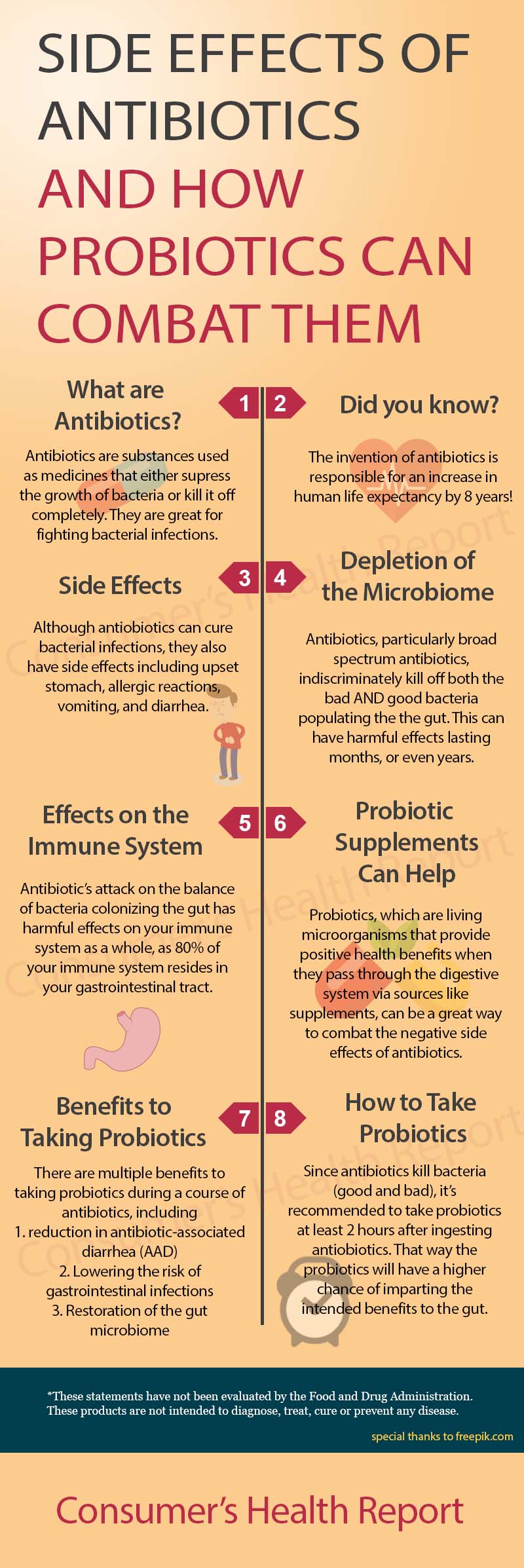
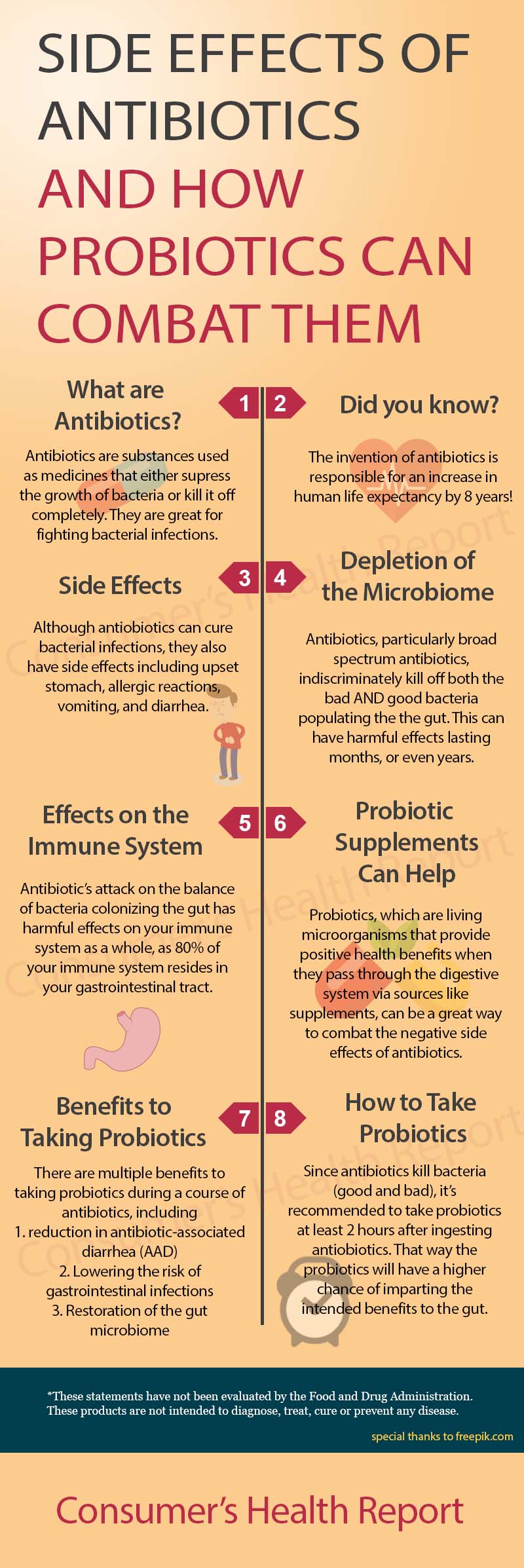
Antibiotics are substances that either suppress the growth of bacteria or kill them completely. [1] Antibiotics revolutionized science and led to an increase of an additional eight years of average life expectancy from 1945 to 1972. [1]
Antibiotics did this by killing bacterial infections that normally would have killed their human host.
Some antibiotics are very specific in what they do and which bacteria they target; these are referred to as “narrow-spectrum” antibiotics. Other forms of antibiotics, called “broad-spectrum”, kill off a wide variety of disease-causing bacteria. Both types of antibiotics can cause problems within the digestive tract, but the latter more so because of their indiscriminate killing of all bacterial forms.
It’s clear that the discovery of antibiotics was a scientific breakthrough, but it didn’t come without its drawbacks.
Issues With Antibiotics
One very concerning issue with antibiotics is their over-prescription.
The Centers for Disease Control published findings in a press release in May of 2016 that one-third of all antibiotic prescriptions are unnecessary. [2] The main reason being that antibiotics are erroneously prescribed to patients with viral illnesses, which do not respond to antibiotics.
The major problem this is leading to is antibiotic-resistant bacteria. There would be far-reaching negative consequences for society without effective antibiotic treatments.
The more concerning issue, however, is that many antibiotics eradicate all bacteria within the digestive tract, both good and bad. In fact, antibiotics affect the gut so severely that “antibiotic-induced microbiota alterations can remain after long periods of time, spanning months and even years”. [3]
This could have harmful effects on the immune system as a whole, considering around “80 percent of your immune system resides in your gastrointestinal tract.” [4]
Antibiotics may be necessary but have side effects that can affect immune system resilience for extended periods of time. Antibiotics should be taken only after determining that it’s absolutely necessary to do so. [42]
What Are Probiotics?
Probiotics are living microorganisms that provide positive health benefits by keeping your digestive system healthy.
There are multiple sources that contain probiotics, the most well-known being in supplements, but they can also be found in some foods, such as yogurt or kimchi. [5]
Many people have the impression that all bacteria are harmful, but that’s not the case when it comes to probiotics.
Probiotics make up part of the “good” bacteria that benefit the digestive system and overall overall health by restoring and/or maintaining bacterial balance. [6]
Do Probiotics Affect Antibiotics and Do They Make Antibiotics Any Less Effective?
Probiotics do not affect antibiotics directly; rather, they provide balance to the composition of the gut microbiome. [7]
The microbiome is the composition of microorganisms that colonize the gut. It is now known that there is a clear bi-directional relationship between these microorganisms and their host that has a significant effect on the host’s health. [41]
Conversely, however, antibiotics can and will kill probiotics if introduced together. After all, antibiotics kill bacteria and that’s what the majority of probiotics are.
Therefore, it’s recommended to take probiotics at least two hours after ingesting antibiotics. [8] That way, the probiotics will have a much higher chance of making the journey through the digestive system alive and be able to pass on the intended benefits.
Not all probiotics are bacteria either. Saccharomyces boulardii is a yeast that has probiotic properties, which makes it an ideal probiotic strain to take when undergoing a course of antibiotic treatment, as it isn’t targeted by antibiotics.
It was also observed to have “significantly increased the eradication rate” [9] of H. pylori, a bacteria that can infect the stomach. [10]
Can You Take Probiotics and Antibiotics at the Same Time?
It’s beneficial to take probiotics throughout a course of treatment but they shouldn’t be taken at the exact same time. As mentioned earlier, p
In a study on the effects of antibiotics on the human gut microbiome, researchers found that the “use of probiotic bacteria aimed at impeding dysbiosis or at reestablishing the gut microbiota after antibiotic treatment is a promising approach.” [3] These are meaningful findings considering that “microbiome alterations induced by antibiotics can also indirectly affect health in the long-term.”
Exposure to antibiotics can cause disruptions within the body’s physiological equilibria, which may increase vulnerabilit to long-term disease. [3]
Researchers from this study also reported that humans today are overexposed to antibiotics not just from taking them but also because of their widespread use in crops and farm animals.
Considering the fact that we’re exposed to antibiotics in some of the meat and other food we consume, consistent use of probiotics to offset some of the negative effects of antibiotics appears to be a viable option.
So to answer the question as to whether probiotics and antibiotics can be taken at the same time, the answer based on the evidence from the scientific literature published thus far is yes. As to why probiotics can and should be taken before, during and after a course of antibiotics, that will be answered in the following section.
Benefits of Taking Probiotics Throughout Antibiotic Treatment
There are several benefits to taking probiotics while on a course of treatment of antibiotics: a reduction in antibiotic-associated diarrhea (AAD), lowering the risk of gastrointestinal infections and restoration of the gut microbiome.
Probiotics and Diarrhea Reduction


Antibiotic-associated diarrhea is estimated to affect up to 30% of all patients who undergo antibiotic treatment and while it’s not a large concern in the majority of patients, it can have serious implications in some instances. [11] Among hospitalized patients suffering from antibiotic-associated diarrhea, there is an increased risk of infections and
In this regard, the discovery and study of probiotics are having some wide-reaching positive implications.
Among the available medical and scientific literature, studies on probiotics showed a decrease in the incidence of antibiotic-associated diarrhea (AAD) among study participants aged 0-65. This is partly why doctors from the University of North Carolina advise fellow doctors to suggest taking probiotics along with their patients’ antibiotics. [13]
In a meta-analysis of the available literature in 2002 on probiotics and antibiotic-associated diarrhea, researchers came to the conclusion that the data suggests that probiotics are effective in the prevention of AAD. However, they were hesitant to make any concrete declarations as to the efficacy of probiotics in the treatment of diarrhea as a result of antibiotics at the time—things have changed since though. [14]
In this 2006 meta-analysis on the treatment of antibiotic-associated diarrhea and
As of 2008, 25 meta-analyses had been conducted on the efficacy of probiotics. Among the studies performed, the “results showed an overall reduction in the risk of AAD when probiotics were coadministered with antibiotics.” [16] The probiotic strains saccharomyces boulardii, lactobacillus gg and bacillus coagulans were deemed to be the most effective.
An article in the Journal for Specialists in Pediatric Nursing entitled ‘Probiotics: Preventing Antibiotic‐Associated Diarrhea’, nurse practitioner Kathleen Jones concluded that “several strains of probiotics are helpful in the prevention and treatment of antibiotic‐associated diarrhea.” [17] As far as practical implications for these findings go, she believes that by understanding the uses, doses and safety of probiotics that nurses and doctors can educate their patients on how probiotics can be beneficial to their health.
In an evidence-based review of probiotics for antibiotic-associated diarrhea and c. diff(clostridium difficile) infections, a PhD from the Department of Health Services Research and Development and the School of Pharmacy at the University of Washington in Seattle, Washington, found that probiotics “offer a promising strategy for the prevention and treatment for AAD and CDI”. [18]
A meta-analysis of randomized controlled trials of the effects of probiotics in children found that probiotics reduced the risk of antibiotic-associated diarrhea from 28.5% to 11.9%. [19]
This study had some different and even more impressive findings: those taking probiotics had a 42 percent lower risk of antibiotic-associated diarrhea. [20]
Another study done on probiotics’ effect on intestinal microbiota/bowel movements used healthy volunteers as its subjects. There were 41 of these test subjects who were taking a treatment course of amoxicillin, one of the most commonly prescribed antibiotics. Of the 41 participants, a portion were given a probiotic supplement to be taken twice daily and the other portion was given a placebo. This study found that probiotics (a multi-strain probiotic was used in this study) modulated the effects of the antibiotic amoxicillin and “significantly reduced” the incidence of
A more thorough and systematic review on probiotics performed in 2012 concluded that probiotics indeed are associated with a reduction of antibiotic-associated diarrhea. With that said, the researchers called for more clinical studies conducted so as to ascertain exactly what strains of probiotics are responsible for preventing and treating AAD and gain a broader understanding of how they should be administered. [11]
Probiotics and Lowered Risk of Gastrointestinal Infections
Probiotics combat pathogens causing gastrointestinal infections in multiple ways: 1) they modify the conditions of the digestive environment, 2) they encourage the production of antimicrobial metabolite and 3) they modulate the immunity mechanisms of the host. [22]
It has been shown across the various meta-analyses carried out that probiotics have generally been shown to be effective in the prevention/treatment of gastrointestinal infections. [23] Among the infections that probiotics prevent and fight against are c.
Clostridium
Additionally, this paper from the Division of Gastroenterology at the University Hospitals of Cleveland reports that clinical trials support the efficacy of probiotics and the prevention of
One very interesting paper reported how long-term consumption of probiotic milk would affect the incidence of infections in children who attend
In a study entitled ‘Effects of probiotics and antibiotics on the intestinal homeostasis in a computer controlled model of the large intestine’, researchers from Germany and the Netherlands found that following the consumption of a probiotic supplement containing 8 strains of probiotics(most notably bifidobacterium breve and lactobacillus acidophilus) combined with a clindamycin therapy “had a beneficial and stabilizing effect on the intestinal metabolic homeostasis by decreasing toxic metabolites and protecting the endogenic microbiota from destruction.”[29] It was also concluded that in regards to achieving/maintaining a healthy balance within the digestive system and keeping intestinal disturbances at bay, that probiotics could be “a reasonable strategy”.
In an article published in the Journal of Medical Microbiology entitled ‘Probiotics to minimize the disruption of
Probiotics and The Gut Microbiome


The medical community has understood the importance of the intestinal microbiota and the role it assumes in the development and function of the gastrointestinal system for some time now.
The microbiota are responsible for “regulating host inflammatory responses and immune homeostasis.”[31]
In other words, when there’s a problem with the intestinal microbiota, it can lead to unnecessary inflammation and a weakened immune system. Not only that, but a convincing amount of evidence has now come to light that the microbiota aids in the regulation of metabolism and sends signals to and interacts with several physiological systems of the host other than just the gastrointestinal system, namely the brain, respiratory tract and urogenital tract.
Mounting evidence has shown that probiotics may “restore the composition of the gut microbiome and introduce beneficial functions to gut microbial communities, resulting in amelioration or prevention of gut inflammation and other intestinal or systemic disease phenotypes.”[32] Considering that antibiotics cause so much negative disruption within the gut, probiotics may be the best way of restoring the natural balance of the microbiota.
As you can imagine, these discoveries have enormous implications for not just weight management but also our overall health as human beings. What the medical and scientific communities ultimately do with this information still remains to be seen but the important takeaway for now is that probiotics have a positive influence over the microbiome and therefore our overall health.
How Much Probiotics Should You Take with Antibiotics?
You should not alter the dosage of probiotics that you normally take while undergoing antibiotic treatment. Following the directions on the label of your probiotics as usual is a good idea.
Antibiotics can kill good probiotic bacteria, which would lead many to believe that more probiotics should be taken to counteract this. However, that’s not necessary, as drug interaction between the two can be avoided by taking probiotics at least 2 hours before or after taking antibiotics.
Are Probiotics Safe to Take While on Antibiotics?
Yes, probiotics are safe to take at any time, whether you’re on a course of antibiotics or not, as long as you’re not suffering from specific health conditions (namely, having a particularly weakened immune system or you’ve recently undergone surgery). [33] Pharmacist Scott Gavura from Science-Based Medicine writes “it is reassuring that there is little evidence in the literature to suggest that probiotics are harmful.” [20]
Should Anyone Avoid Taking Probiotics with Antibiotics?
While probiotics “exhibit an excellent overall safety profile”, they should be avoided for extremely immunocompromised patients(or those taking immunosuppressant medications such as tacrolimus, cyclosporine, azathioprine or chemotherapeutic agents) and premature infants.[34] Examples of of individuals with weakened immune systems include cancer patients, AIDS/HIV patients and those who have inherited diseases that weaken the immune system(congenital agammaglobulinemia or congenital IgA deficiency, for example).[35]
While some say that the risk of probiotic overgrowth is negligible even in immunocompromised persons,
The reason being is that there have been a few documented cases of immunocompromised patients having adverse side effects from certain probiotic strains.[37][38][39]
Should you continue taking probiotics after antibiotics?
Yes. Taking probiotics after antibiotics will help to restore the natural balance of the gut. Probiotics themselves are actually transient(meaning they do not populate the gut and remain there), but they promote healthy composition of the microbiome of the gut and introduce “beneficial functions to gut microbial communities.”[40] The result is that they prevent inflammation/disease and in some cases fight against it.
In other words, antibiotics cause unhealthy disruptions and imbalances in the gut that probiotics can help restore. So taking probiotics after antibiotics is one of the most beneficial times to take them.
Conclusion
We all owe a great deal of gratitude to antibiotics and what they’ve done for society. Many of us wouldn’t even be here today if it weren’t for their ability to kill harmful, pathogenic bacteria.
However, as with many things health-related, there can be too much of a good thing. There are some frightening downsides to both their use and overprescription.
Over-prescription is something that the medical community needs to address; that’s largely outside the control of average consumers. But what we can do as consumers is to put ourselves in the best position to heal properly during and after a course of antibiotics and from the evidence currently available that means taking high-quality, multi-strain probiotics.
See Sources- https://microbiologysociety.org/education-outreach/antibiotics-unearthed/antibiotics-and-antibiotic-resistance/what-are-antibiotics-and-how-do-they-work.html
- https://www.cdc.gov/media/releases/2016/p0503-unnecessary-prescriptions.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709861/
- https://articles.mercola.com/sites/articles/archive/2016/05/17/unnecessary-antibiotic-prescriptions.aspx
- https://www.ncbi.nlm.nih.gov/pubmed/24456350
- https://my.clevelandclinic.org/health/drugs/14598-probiotics
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3539293/
- https://www.medscape.com/viewarticle/719654_13
- https://www.ncbi.nlm.nih.gov/pubmed/25898944
- https://www.mayoclinic.org/diseases-conditions/h-pylori/symptoms-causes/syc-20356171
- https://jamanetwork.com/journals/jama/fullarticle/1151505
- https://journals.lww.com/jcge/Abstract/2008/07001/Probiotics_for_Prevention_of_Antibiotic_associated.4.aspx
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3601687/
- https://www.bmj.com/content/324/7350/1361?lookup=
- https://www.nature.com/articles/ajg2006155
- https://journals.lww.com/jcge/Abstract/2008/07001/Probiotics_for_Prevention_of_Antibiotic_associated.4.aspx
- https://onlinelibrary.wiley.com/doi/full/10.1111/j.1744-6155.2010.00231.x
- https://www.sciencedirect.com/science/article/pii/S1075996409001243#!
- https://www.jpeds.com/article/S0022-3476(06)00383-0/abstract
- https://sciencebasedmedicine.org/ive-been-prescribed-an-antibiotic-should-i-take-a-probiotic/
- https://www.nature.com/articles/ajg20085027
- https://www.ncbi.nlm.nih.gov/pubmed/18221171
- http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0034938
- https://journals.lww.com/co-gastroenterology/Abstract/2005/01000/Probiotic_therapy_of_intestinal_inflammation_and.10.aspx
- https://www.mayoclinic.org/diseases-conditions/c-difficile/symptoms-causes/syc-20351691
- http://www.cochrane.org/CD006095/IBD_use-probiotics-prevent-clostridium-difficile-diarrhea-associated-antibiotic-use
- https://www.ncbi.nlm.nih.gov/pubmed/16524546
- https://www.bmj.com/content/322/7298/1327.full
- https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-12-47
- http://jmm.microbiologyresearch.org/content/journal/jmm/10.1099/jmm.0.47615-0
- https://nyaspubs.onlinelibrary.wiley.com/doi/full/10.1111/nyas.12303
- http://journals.sagepub.com/doi/abs/10.1177/1756283X12459294
- http://hearttoheartmedicalcenter.com/when-probiotics-are-bad-for-you/
- https://www.tandfonline.com/doi/abs/10.1586/eri.12.24?journalCode=ierz20
- https://www.cdc.gov/parasites/crypto/gen_info/infect_ic.html
- https://academic.oup.com/cid/article/36/6/775/319312
- http://jcm.asm.org/content/36/1/325.short
- http://pediatrics.aappublications.org/content/115/1/178.short
- https://www.oncologynurseadvisor.com/oncology-nursing/probiotics-carry-potential-risks-for-immunocompromised/article/719417/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3539293/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4643846/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/